Mycotoxins pose a threat to the horse’s digestive system

Author: Judith Schmidt, Product Manager On Farm Solutions
Alarm in the gut! Horses have a susceptible digestive system that can quickly become unbalanced. Intestinal disorders in horses are usually associated with colic. Many factors can be responsible for intestinal issues. Have you ever thought about mycotoxins? What can horse owners do to support their horse´s gut health?
The equine stomach is not robust at all. Depending on their age and use, more than half of all horses suffer from stomach pain. Their digestive system is very sensitive and very different from that of other mammals: Horses cannot vomit and often suffer from severe abdominal pain, diarrhea, or cramps if they overeat or ingest spoiled feed.
The horse´s digestive system is complex and sensitive
The horse´s stomach has a relatively small capacity of around twelve to fifteen liters. Depending on the feed’s consistency and composition, it remains in the stomach for around one to five hours before it is pressed through the stomach outlet (pylorus) into the small intestine. The horse´s entire intestine is about ten times its body length.
 Figure 1: The horse’s digestive tract
Figure 1: The horse’s digestive tract
The horse´s gastrointestinal tract is a complex network, reacting extremely sensitively to changes and, therefore, highly susceptible to disorders. It essentially consists of the head intestine (lips, oral cavity, teeth, and esophagus), stomach (blind pouch, fundus, and stomach outlet), small intestine (duodenum, jejunum, and ileum), and large intestine (caecum, colon and rectum). Each section plays a crucial role in the digestive process; any disruption can lead to health issues. Understanding this structure is key to maintaining a horse’s digestive health.
Digestive disorders can have various reasons
Intestinal problems in horses can stem from diverse causes, often a complex interplay of multiple factors. By understanding these causes more deeply, horse owners can be better equipped to prevent and manage these issues. In the following, we delve into several of these causes.
1. Too long time between the feedings
Usually, a feeding break should be at most four to six hours, as, in nature, a horse is busy eating for at least 18 hours a day. In contrast to humans, who produce stomach acid only after food intake, the horse’s stomach produces gastric acid around the clock. The continuous intake of roughage, intensive chewing, and high saliva production (a horse produces 5 to 10 L of saliva per day) is, therefore, essential to protect the stomach mucosa by neutralizing excess gastric acid.
A too-long time between feedings and, therefore, no saliva production leads to an accumulation of gastric acid in the stomach. Four hours without roughage can already cause inflammation of the mucosa and probably ulcers.
2. Excessive amounts of concentrated feed
Excessive amounts of concentrates such as wheat or rye, conditioned by less chewing activity, increase gastric acid and histamine production, and the stomach lining can be attacked. Also, in this case, the development of stomach ulcers is possible.
Furthermore, the possibly resulting hyperacidity of the organism can lead to malfunctions of the organs, the skin, and the hooves.
3. Stress
Stress can also lead to a higher production of gastric acid and, therefore, to gastric ulcers. The horse is a flight animal. When it is under stress, it prepares for the impending escape, and the muscles are preferably supplied with blood, resulting in a lower blood flow to the mucous membranes. Furthermore, the rising cortisone level reduces the hydrochloric acid-suppressing prostaglandin E. As a result, more stomach acid is produced, irritating the gastric mucosa.
Stress can be triggered, e.g., by transportation, competitions, training, a change of house, a new rider, unsuitable equipment, or poor posture.
4. Dental diseases
The teeth are essential for digestion. When feed is chewed, it is broken down and mixed with saliva. Chipped teeth cannot chew well, and the feed is not sufficiently salivated or crushed, which has a detrimental effect on digestion.
For this reason, an expert vet should check the horse´s teeth at least once a year.
5. Administration of painkillers/medication
As with humans, long-term medication administration can promote the formation of stomach ulcers. For this reason, it is essential to ensure that horses are fed a gentle diet on the stomach, especially when using oral pain therapy, and to add stomach protection if necessary.
6. Endotoxins
If pathogens such as E. coli or clostridia proliferate extremely or are killed by an antibiotic, endotoxins can be released. These toxins can cause transformation or inflammation of the gut mucosa. In drastic cases, whole areas of the mucosa can die off.
7. Mycotoxins – the hidden danger in horse feed
Mycotoxins in plants and horse feed are a common but often unnoticed danger to horses’ health. Mycotoxins are natural, secondary metabolites of molds that have a toxic effect on humans and animals and can trigger mycotoxicosis. Contaminated feed can severely affect the horse’s health and, in the worst case, lead to death.
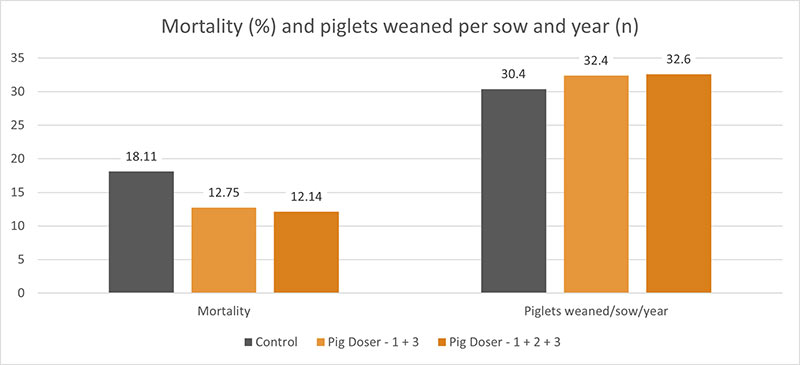
Over 90 % of the world´s feed production is estimated to be contaminated with at least one mycotoxin (see also Global Mycotoxin Report 2023, EW Nutrition. The intake of mycotoxins via hay, grain, silage, or compound feed can hardly be avoided. Mycotoxins are an increasing problem for all horse owners. Scientific studies show that the mycotoxins DON and ZEA are most frequently found in horse feed and, therefore, are also frequently detected in sports horses’ urine and blood samples.
Due to the highly toxic metabolic products, feed contaminated with molds can lead to severe liver and kidney diseases in horses, affect fertility, trigger colic, and promote digestive issues (diarrhea and watery stools).

Figure 2: Mycotoxins and their impact on horses
How to protect the horse from mycotoxins?
The first measure against the ingestion of mycotoxins is prevention. Correct pasture management and adequate barn and feed hygiene can contribute to preventing the ingestion of toxins.
However, despite the best prophylactic measures, it is impossible to prevent mycotoxin contamination of feed completely. As mycotoxins are not visible, analyzing the feed regarding mycotoxin contamination is recommended.
To protect your horse from mycotoxins, EW Nutrition developed MasterRisk, a tool for evaluating the risk of mycotoxins. Additionally, EW Nutrition has developed a complementary feed specifically for your horse´s needs in the form of granules. The sophisticated formulation of “Toxi-Pearls” is designed to bind mycotoxins and mitigate the adverse effects of mycotoxin contamination.
The pearls contain a mixture of mycotoxin binder, brewer’s yeast, and herbs:
- The contained mycotoxin binder effectively controls the most important feed myco- and endotoxins. It additionally supports the liver and immune system and strengthens the intestinal barrier.
- Brewer´s yeast supports the natural strength of the gastrointestinal tract. Due to its high natural content of beta-glucans and mannan-oligosaccharides (MOS), unique surface structure, and the associated high adsorption power, brewer´s yeast has a prebiotic effect on the intestinal microbiome.
- The additional unique herbal mixture consists of the typical gastrointestinal herbs oregano, rosemary, aniseed, fennel, and cinnamon. The processed beetroot is a true all-rounder. Literature shows that it has an antioxidant effect and strengthens the immune system. It also promotes bile secretion and, therefore, supports fat digestion.
Conclusion
The horse’s digestive tract is highly sensitive and must be supported by all means. Besides failures in management, such as too long breaks between feedings or too high amounts of feed concentrate, mycotoxins present a high risk in horse nutrition. To prevent horses from intestinal issues, feed and stress management, dental care, and medication in the case of disease must be optimized. Particular attention should be paid to possible mycotoxin contamination. Effective toxin risk management, which consists of analysis, risk evaluation, and adequate toxin risk-managing products, should be implemented.